Have you ever heard of "lipedema"? Until a few years ago, I hadn't. Yet I quite likely have it, and rather significantly too. I wonder how many other fat women might have it and never realized it's a separate diagnosis from being fat?
However, when I have tried to research the condition, I've been turned off by many lipedema websites. Some pay lip service to being size-friendly but when you dig deeper, there is a whole lot of food neuroses and weight-loss rhetoric, which can be very triggering for those trying to practice Body Love and Health At Every Size®.
After looking around again recently, I decided that it's time for a more size-neutral resource on the topic. Since June is Lipedema Awareness Month, here's a summary of what I've learned about lipedema so far, presented as size-neutrally as possible. I have used a multi-part format for length considerations:
- Part One - Symptoms and appearance of lipedema; lipedema vs. lymphedema
- Part Two - Progression and stages of lipedema
- Part Three - Fat distribution types and diagnostic criteria
- Part Four - Possible causes; conditions often associated with lipedema
- Part Five - Possible treatment options, both traditional and alternative
- Part Six - Practical advice for living and dealing proactively with lipedema, as well as sharing a few women's stories* of lipedema
Terminology
Very few care providers in the US are aware of lipedema. Never has ANY care provider mentioned the possibility of it to me, despite my very distinct symptoms of it.
Lipedema is such an under-recognized condition that until just recently, it did not have a MESH search term in the National Library of Medicine. Nor does it yet have an International Classification of Diseases (ICD) code. The condition was only recognized by the National Health Service (NHS) in the United Kingdom in 2012. Awareness of lipedema is emerging, but very slowly in some quarters.
One problem is terminology. Many care providers confuse lipedema with lymphedema. The spelling and the pronunciation are so similar that it's no wonder many people confuse them. However, while the two conditions can overlap somewhat, they are not the same.
Lipedema is the abnormal deposition of excess fat, usually in the extremities, whereas lymphedema is the collection of protein-rich lymph fluid in tissues, causing swelling.
Lymphedema is pronounced "limf-eh-deem-ah." Lipedema is pronounced "lip-eh-deem-ah." In Europe and Australia they call it "lipoedema" (lye-poh-eh-deem-ah). Terms in the medical literature include:
- Adiposis dolorosa (painful fat syndrome)
- Lipalgia
- Adiposalgia/Adipoalgesia
- Lipomatosis dolorosa of the legs
- Lipohypertrophy dolorosa
- Painful column leg
- Painful lipedema syndrome
- Lipedema (U.S.), lipoedema or lipodema (U.K.), lipödem (Germany)
What is Lipedema?
In layman's terms, lipedema is an abnormal storage and distribution of fat deposits, usually in the lower body but sometimes also in the arms.
Lipedema is considered a R.A.D, a Rare Adipose Disorder. The medical definition, as defined by one source, is:
 Lipedema is characterized by really heavy legs which are bilaterally and symmetrically affected.
Lipedema is characterized by really heavy legs which are bilaterally and symmetrically affected.
Bilateral means BOTH legs are affected (not just one). In the picture to the left, notice that both legs are indeed pretty equally affected.
Symmetrical means the fat deposits are fairly even, not all lumped up in one area. The picture shows this as well. The fat is pretty evenly distributed down the leg until it reaches the ankle, and the two legs look quite alike.
Bilateral and symmetrical means the same even pattern of fat deposition is seen on both legs. That's very important in distinguishing lipedema from lymphedema, as you will see below.
Does Not Involve the Feet
Legs That Lose Their Shape
In early stages of lipedema, there is still some shape to the legs and ankles, but as the condition progresses, the shapeliness of the legs begins to disappear.
Lower legs and ankles start to get thicker and the curves begin to disappear.
Sometimes this is called by the lovely nicknames of "columnar" legs, "piano legs," or "stove-pipe" legs.
This is because as the fat deposition progresses, the leg shape is lost and the legs become more like a column, going mostly straight up and down.
"Cankles On Steroids"
 Society likes to call thick ankles "cankles" (i.e. calf-ankles), but lipedema involves a much more severe presentation ─ basically, cankles on steroids.
Society likes to call thick ankles "cankles" (i.e. calf-ankles), but lipedema involves a much more severe presentation ─ basically, cankles on steroids.
In the early stages of lipedema, the lower legs become slightly thicker than normal but you don't really see cankles.
In the picture to the left, the woman still has shape to her legs but her lower legs are starting to get a bit thicker and you can just begin to see the suggestion of deposits of fat above the ankle. This is an early stage of lipedema.

Little by little (or sometimes in a fairly short period of time in response to a major hormonal change or severe stress), more and more fat begins to be deposited by the ankles.
As the leg becomes more column-like and less curvy, a "stepped" appearance from the feet to the legs begins to appear.
As some doctors describe a "stepped" appearance, if you ran your hands around the feet and then up to the ankles your hand would get stuck momentarily by the increase of fat at or just above the ankles. You would not have a smooth transition from the foot to the leg because of the significant increase at the ankles.
 As lipedema progresses, it often looks like you've worn socks that were too tight and this has left a ring on the skin. This "ring" around the ankles is a classic sign of middle-stage lipedema. If you look carefully, you can see that "ring" in these two pictures.
As lipedema progresses, it often looks like you've worn socks that were too tight and this has left a ring on the skin. This "ring" around the ankles is a classic sign of middle-stage lipedema. If you look carefully, you can see that "ring" in these two pictures.
In time many women with lipedema develop a bump of fat just above the ankles, as you can see in this close-up just above the "ring." This is what gives the leg the "stepped" appearance.
Lymphedema is much different than lipedema. Lipedema is caused by the abnormal deposition of fatty tissue. Lymphedema has to do with impaired flow of lymph fluid and the resulting swelling.
Again, although people with latter-stage lipedema often develop lymphedema as a complication because fatty deposits can impair lymph flow, the reverse is never true ─ people with lymphedema do not develop lipedema as a complication.
One definition of lymphedema can be found here:
 In contrast to lipedema, lymphedema affects feet as well as legs, as can be observed in the picture to the left. This is one of the most important ways to distinguish between the two conditions.
In contrast to lipedema, lymphedema affects feet as well as legs, as can be observed in the picture to the left. This is one of the most important ways to distinguish between the two conditions.
In lymphedema, the swelling often starts in the toes and continues upwards, whereas with lipedema the fat deposits start near the waist and extend downwards to the ankles.
Occasionally, lipedema patients will also have swelling of the feet, but typically this only happens with either temporary lymphedema due to trauma like surgery, or when secondary lipo-lymphedema has developed.
Onset during puberty is common with lipedema, whereas with lymphedema, onset can occur at any age. Lymphedema is often seen after major cancer surgeries, for example, when the lymph system has been damaged.
Another important difference is that lymphedema often affects only one limb, and is usually not symmetrical all over. Note in the picture to the left the difference in size between the leg. Notice also that one foot is swollen and the other is not. This is clearly lymphedema.
Sometimes lymphedema does involve both legs, but that's unusual, and if it happens, the pattern of swelling almost always involves the feet.
.
 Here is another picture of a lymphedema case. Notice that only one leg is affected, and there is a huge difference in size between the two legs. Notice also that while there is "overshouldering" of the ankle on the affected leg, the foot is also affected and is much larger than the foot on the other leg. Nor does the skin have the characteristic "orange peel" or "mattress skin" look that you would expect if the leg on the right were truly from lipedema.
Here is another picture of a lymphedema case. Notice that only one leg is affected, and there is a huge difference in size between the two legs. Notice also that while there is "overshouldering" of the ankle on the affected leg, the foot is also affected and is much larger than the foot on the other leg. Nor does the skin have the characteristic "orange peel" or "mattress skin" look that you would expect if the leg on the right were truly from lipedema.
Lymphedema can occur in males or females, whereas lipedema is usually limited to females. There is no increased bruising with lymphedema, and the skin texture is harder or more fibrotic, while it is more rubbery with lipedema. Sometimes there are changes in skin color with lymphedema, whereas this is less common with lipedema (unless secondary lymphedema or an infection has developed).
Blogs, Websites, and Facebook Pages from Those Dealing with LipedemaIn layman's terms, lipedema is an abnormal storage and distribution of fat deposits, usually in the lower body but sometimes also in the arms.
Lipedema is considered a R.A.D, a Rare Adipose Disorder. The medical definition, as defined by one source, is:
A chronically progressive, symmetrical accumulation of fat in the subcutaneous tissue with orthostatic edema occurring almost exclusively in women.Wikipedia defines it as:
...a chronic disorder of adipose tissue generally affecting the legs, which causes the legs and sometimes the arms to accumulate fatty tissue.Once in a while it's called "Riding Breeches Syndrome." Some women have described it as like being held prisoner inside a fat suit on their lower body, a fat suit shaped like pantaloons (when the leg to the ankle is affected) or riding breeches (when the waist to the knees is affected).
According to Rebecca Morris, the founding president of the National Lipedema Association (NLA), lipedema is distinctive in four ways:
- It can be inherited
- It occurs almost exclusively in women
- It occurs in women of all sizes, from the anorexic to the very heavy
- Lipedemic fat generally is not mobilized by diet and exercise
Wikipedia adds two more defining characteristics:
- It involves the excess deposit and expansion of fat cells in an unusual and particular pattern – bilateral, symmetrical and usually from the waist to a distinct line just above the ankles
- a pathognomonic [definitive] indicator of lipedema is that the feet are spared
What Does Lipedema Look Like?
Here are some pictures to help illustrate the most important characteristics of lipedema. Be warned ─ pictures of the more severe presentations are hard to look at.
Don't panic; remember that not everyone progresses to the severe stages and that even if you do, treatment is available. The pictures merely serve as warning of why early diagnosis and effective treatment are so important.
Disproportionate Body
In the beginning, lipedema is often just a significantly disproportionate "pear" shape. Often women wear a different size on top than on the bottom.
One part of the body (often the hips and upper thighs at first) tends to be much larger than the rest of the body, as in the picture to the left. Some people think of this as "thunder thighs" but it's more than just legs that rub together a bit.
As time goes on, more and more fat begins to be preferentially deposited in the legs and hips. Often the area around the knees begins to develop extra fat pads, and the area just above the ankles starts to get thicker. If you look closely at the picture on the left, you can see the beginnings of these deposits.
In lipedema, the lower half of the body typically is disproportionately larger than the rest of the body and can become even more disproportionate with time.
There are some exceptions to this; some women with lipedema also have significantly larger arms and sometimes chest too. Sometimes there's a lot of fat between the waist and the knees but the lower legs are not nearly as affected. However, the majority of women with lipedema start off with the classic "pear" shape and a lower body that is larger than the rest of her body.
Bilateral and Symmetrical
Here are some pictures to help illustrate the most important characteristics of lipedema. Be warned ─ pictures of the more severe presentations are hard to look at.
Don't panic; remember that not everyone progresses to the severe stages and that even if you do, treatment is available. The pictures merely serve as warning of why early diagnosis and effective treatment are so important.
Disproportionate Body
In the beginning, lipedema is often just a significantly disproportionate "pear" shape. Often women wear a different size on top than on the bottom.
One part of the body (often the hips and upper thighs at first) tends to be much larger than the rest of the body, as in the picture to the left. Some people think of this as "thunder thighs" but it's more than just legs that rub together a bit.
As time goes on, more and more fat begins to be preferentially deposited in the legs and hips. Often the area around the knees begins to develop extra fat pads, and the area just above the ankles starts to get thicker. If you look closely at the picture on the left, you can see the beginnings of these deposits.
In lipedema, the lower half of the body typically is disproportionately larger than the rest of the body and can become even more disproportionate with time.
There are some exceptions to this; some women with lipedema also have significantly larger arms and sometimes chest too. Sometimes there's a lot of fat between the waist and the knees but the lower legs are not nearly as affected. However, the majority of women with lipedema start off with the classic "pear" shape and a lower body that is larger than the rest of her body.
Bilateral and Symmetrical
 Lipedema is characterized by really heavy legs which are bilaterally and symmetrically affected.
Lipedema is characterized by really heavy legs which are bilaterally and symmetrically affected. Bilateral means BOTH legs are affected (not just one). In the picture to the left, notice that both legs are indeed pretty equally affected.
Symmetrical means the fat deposits are fairly even, not all lumped up in one area. The picture shows this as well. The fat is pretty evenly distributed down the leg until it reaches the ankle, and the two legs look quite alike.
Bilateral and symmetrical means the same even pattern of fat deposition is seen on both legs. That's very important in distinguishing lipedema from lymphedema, as you will see below.
Does Not Involve the Feet
One of the most defining characteristics of lipedema is that it ends at the ankle and does NOT involve the feet.
It's not just fat legs; it's disproportionately fat legs without fat feet too.
It's not just fat legs; it's disproportionately fat legs without fat feet too.
Notice that the legs in the picture fit the description. Both legs are affected pretty equally and evenly (bilateral and symmetrical), but the feet are not affected. That's one of the key symptoms doctors will look for when diagnosing lipedema.
However, it should be noted that if severe secondary lymphedema develops, sometimes the feet can also develop swelling. Thus, in the early to middle stages of lipedema, feet will not be affected, but in the later stages, feet can sometimes be affected too.
However, it should be noted that if severe secondary lymphedema develops, sometimes the feet can also develop swelling. Thus, in the early to middle stages of lipedema, feet will not be affected, but in the later stages, feet can sometimes be affected too.
Legs That Lose Their Shape
In early stages of lipedema, there is still some shape to the legs and ankles, but as the condition progresses, the shapeliness of the legs begins to disappear.
Lower legs and ankles start to get thicker and the curves begin to disappear.
Sometimes this is called by the lovely nicknames of "columnar" legs, "piano legs," or "stove-pipe" legs.
This is because as the fat deposition progresses, the leg shape is lost and the legs become more like a column, going mostly straight up and down.
"Cankles On Steroids"
 Society likes to call thick ankles "cankles" (i.e. calf-ankles), but lipedema involves a much more severe presentation ─ basically, cankles on steroids.
Society likes to call thick ankles "cankles" (i.e. calf-ankles), but lipedema involves a much more severe presentation ─ basically, cankles on steroids.In the early stages of lipedema, the lower legs become slightly thicker than normal but you don't really see cankles.
In the picture to the left, the woman still has shape to her legs but her lower legs are starting to get a bit thicker and you can just begin to see the suggestion of deposits of fat above the ankle. This is an early stage of lipedema.

Little by little (or sometimes in a fairly short period of time in response to a major hormonal change or severe stress), more and more fat begins to be deposited by the ankles.
As the leg becomes more column-like and less curvy, a "stepped" appearance from the feet to the legs begins to appear.
As some doctors describe a "stepped" appearance, if you ran your hands around the feet and then up to the ankles your hand would get stuck momentarily by the increase of fat at or just above the ankles. You would not have a smooth transition from the foot to the leg because of the significant increase at the ankles.
 As lipedema progresses, it often looks like you've worn socks that were too tight and this has left a ring on the skin. This "ring" around the ankles is a classic sign of middle-stage lipedema. If you look carefully, you can see that "ring" in these two pictures.
As lipedema progresses, it often looks like you've worn socks that were too tight and this has left a ring on the skin. This "ring" around the ankles is a classic sign of middle-stage lipedema. If you look carefully, you can see that "ring" in these two pictures.In time many women with lipedema develop a bump of fat just above the ankles, as you can see in this close-up just above the "ring." This is what gives the leg the "stepped" appearance.
In the later stages of lipedema, the bump gets large enough that it is very distinctive. Many lipedema resources talk about this characteristic "bracelet" of fat just above the ankles on both legs. Some doctors call this bracelet of fat "inverse shouldering" or "overshouldering."
As the condition worsens, the shape of the ankles begins to disappear. Eventually, the "shoulders" droop down to hang over the ankles.
This makes it extremely difficult to get socks or boots that fit.
When it's severe, the "overshouldering" of the ankles can droop way down past the ankles. Sometimes the swelling extends nearly to the floor. The skin can become quite prone to infections.
In the picture to the left, the woman obviously has developed secondary lymphedema and her legs are severely affected. However, note that the feet are not involved and that both legs are pretty equally affected. This is probably lipo-lymphedema rather than straight lymphedema. At this point, it really is like having a "pantaloon" fat suit over your legs.
Obviously, this is an extreme stage and most women with lipidema do not experience this level of overshouldering. At this point, some major Manual Lymph Drainage treatment and compression wrapping is needed to reduce the size of the ankles and legs and to restore comfortable functioning.
"Mattress" Skin
 In lipedema, the skin starts smooth in the early stages, but as the condition progresses, the skin often develops an appearance some people compare to cottage cheese, a mattress, or an orange peel, as in this picture. Beneath the skin, you may feel little nodules or lumps of fat that feel like little peas or beans under the skin. As the condition progresses, these may start to feel larger. This is probably what causes the "cottage cheese" appearance.
In lipedema, the skin starts smooth in the early stages, but as the condition progresses, the skin often develops an appearance some people compare to cottage cheese, a mattress, or an orange peel, as in this picture. Beneath the skin, you may feel little nodules or lumps of fat that feel like little peas or beans under the skin. As the condition progresses, these may start to feel larger. This is probably what causes the "cottage cheese" appearance.
Big Hips, Behind, and Abdomen
Although lipedema is usually thought of as happening primarily in the legs, it can occur from the waist down (including abdomen and hips).
Often the person has a lot of "junk in the trunk," with a very large behind. Sometimes it tends to jut out and become what some people crudely call a "shelf butt." Or the lower abdomen can grow quite large, especially with repeated bouts of weight loss/weight regain, after pregnancy, or with secondary lymphedema.
This can make finding clothes very difficult. Often, women must purchase pants that are far too large in the waist in order to find some that fit in the hips, abdomen, or thighs.
Arms Can Be Affected Too
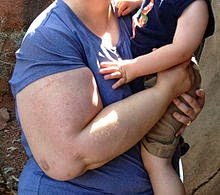
Sometimes the arms develop lipedema too. One well-known expert in the field states that about 30% of people with lipedema also have arms that are affected.
In the picture to the left, notice that the upper arm is very heavy but that the lower arm is not. This is a common lipedema pattern.
These extremely heavy upper arms can make it very difficult to find shirts that fit. Shirts that are wide enough to fit the upper arms are often far too loose on lower arms. Most short-sleeve shirts don't begin to cover the whole upper arm and can cut uncomfortably into the arm.
 The proximity of the arms to the face means that upper-body lipedema is more noticeable to others, and women with affected arms often get more remarks and negative attention. Heavy legs can be covered up by loose pants and long skirts, but lipedema arms are more noticeable, covered or not.
The proximity of the arms to the face means that upper-body lipedema is more noticeable to others, and women with affected arms often get more remarks and negative attention. Heavy legs can be covered up by loose pants and long skirts, but lipedema arms are more noticeable, covered or not.
Although most women with arm lipedema experience it only in the upper arm, sometimes the lower arm is heavy too, as in this second arm picture. In these cases, the "bracelet of fat" that is usually seen around the ankle can also be seen around the wrist, as in the picture.
Interestingly, for whatever reason, in lipedema the arms do not usually develop the typical "cottage cheese" skin texture as badly as the legs often do. They can have the nodules of fat that the legs get, but they may not be as noticeable.
Folds and Ridges of Fat
As lipedema worsens, more and more fat is deposited on the legs. This begins to deform the leg in different ways with harmful side effects.
Frequently there is a big pad of fat on the inside of the knees, as in the picture to the left. This can begin to alter the woman's gait; an altered gait can in turn lead to issues with the feet, hips, and back.
The extra fat pads and altered gait can make exercise more difficult and painful, leading to decreased fitness as the lipedema worsens.
In addition, fluids from the abnormal fat deposits can leak into the knee itself, making it very prone to arthritis at earlier ages than normal. This, too, increases the pain associated with exercise and makes it difficult to keep up fitness.
 In time, large lumps, folds, and ridges can begin to appear. Often these folds and ridges develop around the knees first.
In time, large lumps, folds, and ridges can begin to appear. Often these folds and ridges develop around the knees first.
It is very common to develop a mound of fat tissue just below the knees, as you see in the picture to the left. Notice there is also some folds and ridges of fat above the knee as well. The upper leg has the classic orange peel look, and the abdomen is also enlarged.
This picture shows a variation in lipedema in that there is less of the typical bracelet of fat around the ankles. This woman has a slightly different type of lipedema, the "riding breeches" version, where the excess fat extends from the waist down to just below the knee and mostly spares the ankles. Anecdotally, this type seems to be particularly prone to secondary lymphedema.
As lipedema progresses into more severe stages, even larger masses of tissue can develop and the leg can become quite large.
This woman probably also has the "riding breeches" form of lipedema that is heaviest from waist to just below the knee. She does have a small bracelet of fat around the ankle, but she is much larger in the abdomen and top two-thirds of her leg.
Secondary lymphedema has developed here, causing additional folds and ridges of fat to appear. Notice the fold on the outside above the knee, the fold and ridge below the knee, the fold on the inner thigh, and the "saddlebag" fold near where the hip and thigh meet. This kind of deformation is common with lipo-lymphedema and can often be reduced considerably with treatment.
Summary
Lipedema presents with certain key characteristics, including a disproportionate body shape, bilateral and symmetrical fat deposition on the legs, dimpled "mattress" skin, and a bracelet of fat around the ankle in many (but not all) cases. Probably the most definitive characteristic of lipedema is the lack of involvement of the foot. This is one feature that doctors particularly look for when trying to differentiate lipedema from other possible diagnoses.
If lipedema worsens, folds and ridges of fat can occur. If secondary lymphedema develops, these can become extremely large, severely deforming the leg and making it difficult to walk. Sometimes the lymphedema also spreads into the foot at this stage.
The good news is that treatment may be able to help slow down or even prevent progression of the condition into lipo-lymphedema.
Other Symptoms of Lipedema
Although the strongest characteristics of lipedema are the ones described above, there are other symptoms commonly found among many people with lipedema. These include:
Pain in the Legs
One classic sign of lipedema (but not lymphedema) is high sensitivity to pain with even minimal pressure on the legs, especially on the shins and calves. This sensitivity to touch does not extend to the whole body. Lower leg massage may be too painful, but massage on the back is fine (unless there is fibromyalgia). The pin-point pressure of a cat walking up the leg can cause extreme pain, whereas the same cat walking on the abdomen is fine.
In addition, many women with lipedema report a deep, aching pain from inside the legs, which is why it is sometimes called Painful Fat Syndrome. Some sources believe that this is a separate condition (Dercum's Disease), while others believe that it is part of the spectrum of lipedema. But because Dercum's Disease can occur in several places in the body and onset is usually around menopause (lipedema mostly occurs in the lower body and onset is usually puberty), they are usually considered separate conditions.
Easy Bruising
Many women with lipedema experience cold legs and feet (hypothermia of the skin), although this symptom tends to get overlooked a lot. The woman may have cold feet or legs even when others around her are comfortable, or the skin on her legs may be much colder than on her upper body. This can be a significant source of discomfort for some.
Anecdotally, some women find that it takes significant outside heat sources (hot pads, other people, etc.) to warm up their feet or legs in cold weather. The best guess is that the increased adiposity in the legs interferes with blood and lymph flow, making it harder to regulate temperature.
Swelling
Many women with lipedema experience swelling in the extremities during hot weather or after a long day on their feet. They may find that their fingers swell so much during a walk on a hot summer's day that they cannot tolerate wearing rings at all in the summer.
At first, this swelling resolves pretty easily with rest and elevation, but as lipedema progresses, the swelling tends to not resolve as well due to the lymph system becoming increasingly compromised.
Spider and Varicose Veins
Spider veins and varicose veins are also common in people with lipedema. Spider veins ("telangiectasias") are tiny red veins you can see on the surface of the legs. This is probably due to damage to capillary blood vessels. Varicose veins are also often found.
Unexplained Weight Gain
Many women with lipedema have a history of large, unexplained weight gains, especially associated with major hormonal changes (puberty, pregnancy, perimenopause, and perhaps hormonal birth control) or stress (which increases cortisol and can trigger an inflammation cascade).
Some experience sudden weight or fat gains even when their habits have not changed. Sometimes this gain is mild, sometimes it is extreme. Often it occurs despite aggressive attempts to stop it via diet and exercise.
Difficulty Losing Weight
Many women with lipedema have great difficulty losing weight, especially in the lower half of their bodies. Most have tried very hard to diet away the extra fat. Sometimes weight loss occurs, but is lower in amount than what would be expected by caloric count, and it often returns with a vengeance afterwards. Some even gain weight while on a diet and stringent exercise plan.
Even when weight is lost in the upper body, very little is lost in the lower body, including after bariatric surgery like gastric bypass. All this suggests strongly that there is something going on here beyond simplistic "calories in, calories out" calculations.
Summary
All of this is part of the symptom spectrum of lipedema. You don't have to have all of these symptoms to have lipedema, but if you have most of them, you probably have lipedema. If in doubt, consult your doctor ─ just make sure he/she is well-educated about lipedema first so you can get an accurate evaluation.
This makes it extremely difficult to get socks or boots that fit.
When it's severe, the "overshouldering" of the ankles can droop way down past the ankles. Sometimes the swelling extends nearly to the floor. The skin can become quite prone to infections.
In the picture to the left, the woman obviously has developed secondary lymphedema and her legs are severely affected. However, note that the feet are not involved and that both legs are pretty equally affected. This is probably lipo-lymphedema rather than straight lymphedema. At this point, it really is like having a "pantaloon" fat suit over your legs.
Obviously, this is an extreme stage and most women with lipidema do not experience this level of overshouldering. At this point, some major Manual Lymph Drainage treatment and compression wrapping is needed to reduce the size of the ankles and legs and to restore comfortable functioning.
"Mattress" Skin
 In lipedema, the skin starts smooth in the early stages, but as the condition progresses, the skin often develops an appearance some people compare to cottage cheese, a mattress, or an orange peel, as in this picture. Beneath the skin, you may feel little nodules or lumps of fat that feel like little peas or beans under the skin. As the condition progresses, these may start to feel larger. This is probably what causes the "cottage cheese" appearance.
In lipedema, the skin starts smooth in the early stages, but as the condition progresses, the skin often develops an appearance some people compare to cottage cheese, a mattress, or an orange peel, as in this picture. Beneath the skin, you may feel little nodules or lumps of fat that feel like little peas or beans under the skin. As the condition progresses, these may start to feel larger. This is probably what causes the "cottage cheese" appearance.Big Hips, Behind, and Abdomen
Although lipedema is usually thought of as happening primarily in the legs, it can occur from the waist down (including abdomen and hips).
Often the person has a lot of "junk in the trunk," with a very large behind. Sometimes it tends to jut out and become what some people crudely call a "shelf butt." Or the lower abdomen can grow quite large, especially with repeated bouts of weight loss/weight regain, after pregnancy, or with secondary lymphedema.
This can make finding clothes very difficult. Often, women must purchase pants that are far too large in the waist in order to find some that fit in the hips, abdomen, or thighs.
Arms Can Be Affected Too
Sometimes the arms develop lipedema too. One well-known expert in the field states that about 30% of people with lipedema also have arms that are affected.
In the picture to the left, notice that the upper arm is very heavy but that the lower arm is not. This is a common lipedema pattern.
These extremely heavy upper arms can make it very difficult to find shirts that fit. Shirts that are wide enough to fit the upper arms are often far too loose on lower arms. Most short-sleeve shirts don't begin to cover the whole upper arm and can cut uncomfortably into the arm.
 The proximity of the arms to the face means that upper-body lipedema is more noticeable to others, and women with affected arms often get more remarks and negative attention. Heavy legs can be covered up by loose pants and long skirts, but lipedema arms are more noticeable, covered or not.
The proximity of the arms to the face means that upper-body lipedema is more noticeable to others, and women with affected arms often get more remarks and negative attention. Heavy legs can be covered up by loose pants and long skirts, but lipedema arms are more noticeable, covered or not.Although most women with arm lipedema experience it only in the upper arm, sometimes the lower arm is heavy too, as in this second arm picture. In these cases, the "bracelet of fat" that is usually seen around the ankle can also be seen around the wrist, as in the picture.
Interestingly, for whatever reason, in lipedema the arms do not usually develop the typical "cottage cheese" skin texture as badly as the legs often do. They can have the nodules of fat that the legs get, but they may not be as noticeable.
Frequently there is a big pad of fat on the inside of the knees, as in the picture to the left. This can begin to alter the woman's gait; an altered gait can in turn lead to issues with the feet, hips, and back.
The extra fat pads and altered gait can make exercise more difficult and painful, leading to decreased fitness as the lipedema worsens.
In addition, fluids from the abnormal fat deposits can leak into the knee itself, making it very prone to arthritis at earlier ages than normal. This, too, increases the pain associated with exercise and makes it difficult to keep up fitness.
 In time, large lumps, folds, and ridges can begin to appear. Often these folds and ridges develop around the knees first.
In time, large lumps, folds, and ridges can begin to appear. Often these folds and ridges develop around the knees first.It is very common to develop a mound of fat tissue just below the knees, as you see in the picture to the left. Notice there is also some folds and ridges of fat above the knee as well. The upper leg has the classic orange peel look, and the abdomen is also enlarged.
This picture shows a variation in lipedema in that there is less of the typical bracelet of fat around the ankles. This woman has a slightly different type of lipedema, the "riding breeches" version, where the excess fat extends from the waist down to just below the knee and mostly spares the ankles. Anecdotally, this type seems to be particularly prone to secondary lymphedema.
This woman probably also has the "riding breeches" form of lipedema that is heaviest from waist to just below the knee. She does have a small bracelet of fat around the ankle, but she is much larger in the abdomen and top two-thirds of her leg.
Secondary lymphedema has developed here, causing additional folds and ridges of fat to appear. Notice the fold on the outside above the knee, the fold and ridge below the knee, the fold on the inner thigh, and the "saddlebag" fold near where the hip and thigh meet. This kind of deformation is common with lipo-lymphedema and can often be reduced considerably with treatment.
Summary
Lipedema presents with certain key characteristics, including a disproportionate body shape, bilateral and symmetrical fat deposition on the legs, dimpled "mattress" skin, and a bracelet of fat around the ankle in many (but not all) cases. Probably the most definitive characteristic of lipedema is the lack of involvement of the foot. This is one feature that doctors particularly look for when trying to differentiate lipedema from other possible diagnoses.
If lipedema worsens, folds and ridges of fat can occur. If secondary lymphedema develops, these can become extremely large, severely deforming the leg and making it difficult to walk. Sometimes the lymphedema also spreads into the foot at this stage.
The good news is that treatment may be able to help slow down or even prevent progression of the condition into lipo-lymphedema.
Other Symptoms of Lipedema
Although the strongest characteristics of lipedema are the ones described above, there are other symptoms commonly found among many people with lipedema. These include:
- High sensitivity to pain in the legs
- Tendency towards easy bruising on the legs
- Cold legs and feet
- Edema/swelling at times
- Spider veins/varicose veins
- Tendency towards unexplained weight gain
- Difficulty losing weight, especially in the lower body
Let's discuss each one of these a bit more closely.
One classic sign of lipedema (but not lymphedema) is high sensitivity to pain with even minimal pressure on the legs, especially on the shins and calves. This sensitivity to touch does not extend to the whole body. Lower leg massage may be too painful, but massage on the back is fine (unless there is fibromyalgia). The pin-point pressure of a cat walking up the leg can cause extreme pain, whereas the same cat walking on the abdomen is fine.
In addition, many women with lipedema report a deep, aching pain from inside the legs, which is why it is sometimes called Painful Fat Syndrome. Some sources believe that this is a separate condition (Dercum's Disease), while others believe that it is part of the spectrum of lipedema. But because Dercum's Disease can occur in several places in the body and onset is usually around menopause (lipedema mostly occurs in the lower body and onset is usually puberty), they are usually considered separate conditions.
Easy Bruising
People with lipedema also tend to bruise easily due to increased capillary fragility. Although women with lipedema are not usually covered in bruises, they do tend to bruise more easily than others, and often have bruises on their legs they can't explain away easily.
Cold Legs and Feet
Cold Legs and Feet
Many women with lipedema experience cold legs and feet (hypothermia of the skin), although this symptom tends to get overlooked a lot. The woman may have cold feet or legs even when others around her are comfortable, or the skin on her legs may be much colder than on her upper body. This can be a significant source of discomfort for some.
Anecdotally, some women find that it takes significant outside heat sources (hot pads, other people, etc.) to warm up their feet or legs in cold weather. The best guess is that the increased adiposity in the legs interferes with blood and lymph flow, making it harder to regulate temperature.
Swelling
Many women with lipedema experience swelling in the extremities during hot weather or after a long day on their feet. They may find that their fingers swell so much during a walk on a hot summer's day that they cannot tolerate wearing rings at all in the summer.
At first, this swelling resolves pretty easily with rest and elevation, but as lipedema progresses, the swelling tends to not resolve as well due to the lymph system becoming increasingly compromised.
Spider and Varicose Veins
Spider veins and varicose veins are also common in people with lipedema. Spider veins ("telangiectasias") are tiny red veins you can see on the surface of the legs. This is probably due to damage to capillary blood vessels. Varicose veins are also often found.
Unexplained Weight Gain
Many women with lipedema have a history of large, unexplained weight gains, especially associated with major hormonal changes (puberty, pregnancy, perimenopause, and perhaps hormonal birth control) or stress (which increases cortisol and can trigger an inflammation cascade).
Some experience sudden weight or fat gains even when their habits have not changed. Sometimes this gain is mild, sometimes it is extreme. Often it occurs despite aggressive attempts to stop it via diet and exercise.
Difficulty Losing Weight
Many women with lipedema have great difficulty losing weight, especially in the lower half of their bodies. Most have tried very hard to diet away the extra fat. Sometimes weight loss occurs, but is lower in amount than what would be expected by caloric count, and it often returns with a vengeance afterwards. Some even gain weight while on a diet and stringent exercise plan.
Even when weight is lost in the upper body, very little is lost in the lower body, including after bariatric surgery like gastric bypass. All this suggests strongly that there is something going on here beyond simplistic "calories in, calories out" calculations.
Summary
All of this is part of the symptom spectrum of lipedema. You don't have to have all of these symptoms to have lipedema, but if you have most of them, you probably have lipedema. If in doubt, consult your doctor ─ just make sure he/she is well-educated about lipedema first so you can get an accurate evaluation.
Lipedema vs. Lymphedema
Lymphedema is much different than lipedema. Lipedema is caused by the abnormal deposition of fatty tissue. Lymphedema has to do with impaired flow of lymph fluid and the resulting swelling.
Again, although people with latter-stage lipedema often develop lymphedema as a complication because fatty deposits can impair lymph flow, the reverse is never true ─ people with lymphedema do not develop lipedema as a complication.
One definition of lymphedema can be found here:
Lymphedema is an accumulation of lymphatic fluid in the interstitial tissue that causes swelling, most often in the arm(s) and/or leg(s), and occasionally in other parts of the body. Lymphedema can develop when lymphatic vessels are missing or impaired (primary), or when lymph vessels are damaged or lymph nodes removed (secondary).
When the impairment becomes so great that the lymphatic fluid exceeds the lymphatic transport capacity, an abnormal amount of protein-rich fluid collects in the tissues of the affected area. Left untreated, this stagnant, protein-rich fluid not only causes tissue channels to increase in size and number, but also reduces oxygen availability in the transport system, interferes with wound healing, and provides a culture medium for bacteria that can result in lymphangitis (infection).
 In contrast to lipedema, lymphedema affects feet as well as legs, as can be observed in the picture to the left. This is one of the most important ways to distinguish between the two conditions.
In contrast to lipedema, lymphedema affects feet as well as legs, as can be observed in the picture to the left. This is one of the most important ways to distinguish between the two conditions.In lymphedema, the swelling often starts in the toes and continues upwards, whereas with lipedema the fat deposits start near the waist and extend downwards to the ankles.
Occasionally, lipedema patients will also have swelling of the feet, but typically this only happens with either temporary lymphedema due to trauma like surgery, or when secondary lipo-lymphedema has developed.
Onset during puberty is common with lipedema, whereas with lymphedema, onset can occur at any age. Lymphedema is often seen after major cancer surgeries, for example, when the lymph system has been damaged.
Another important difference is that lymphedema often affects only one limb, and is usually not symmetrical all over. Note in the picture to the left the difference in size between the leg. Notice also that one foot is swollen and the other is not. This is clearly lymphedema.
Sometimes lymphedema does involve both legs, but that's unusual, and if it happens, the pattern of swelling almost always involves the feet.
.
 Here is another picture of a lymphedema case. Notice that only one leg is affected, and there is a huge difference in size between the two legs. Notice also that while there is "overshouldering" of the ankle on the affected leg, the foot is also affected and is much larger than the foot on the other leg. Nor does the skin have the characteristic "orange peel" or "mattress skin" look that you would expect if the leg on the right were truly from lipedema.
Here is another picture of a lymphedema case. Notice that only one leg is affected, and there is a huge difference in size between the two legs. Notice also that while there is "overshouldering" of the ankle on the affected leg, the foot is also affected and is much larger than the foot on the other leg. Nor does the skin have the characteristic "orange peel" or "mattress skin" look that you would expect if the leg on the right were truly from lipedema.Lymphedema can occur in males or females, whereas lipedema is usually limited to females. There is no increased bruising with lymphedema, and the skin texture is harder or more fibrotic, while it is more rubbery with lipedema. Sometimes there are changes in skin color with lymphedema, whereas this is less common with lipedema (unless secondary lymphedema or an infection has developed).
In addition, people with lymphedema may get pitting edema (where you press down the skin and it stays down), as seen in the picture to the left. Pitting edema is rare in lipedema, however, unless secondary lipo-lymphedema has also developed.
Abnormal retention of fluid and difficulty moving lymph is part of both syndromes. In lymphedema, it's usually caused by trauma to the area (like surgery, radiation, chemotherapy) or from vascular anomalies.
In lipedema, lymph issues are caused by the abnormal deposition of fat cells blocking lymph flow. As noted, this causes severe swelling and deforming ridges and folds of fat.
Notice that while the woman on the left clearly has lymphedema, both legs are affected, the feet are much smaller, and there are characteristic fat pads at the knees and over-shouldering around the ankles. This is a LIPEDEMA patient who has also developed secondary lipo-lymphedema.
When lipedema patients develop significant secondary lymphedema, it can become very extreme and debilitating, even life-threatening. The goal of diagnosis and treatment of lipedema is to keep it from progressing to these severe stages.
Summary
Lipedema was first described in the medical literature in 1940 by Doctors Allen and Hines of the Mayo Clinic. However, it did not become well-known among U.S. providers. European providers were also slow to recognize lipedema, but generally have more awareness of it today than U.S. providers. Many countries outside of Europe and the U.S. have even less awareness of it.
One important point is that we do not truly know how common lipedema is. It is called a "Rare Adipose Disorder" but it is probably not that rare. The Lipoedema Australia Support Society (LASS) says that 5-15% of women may have it. One epidemiological study estimated that about 11% of women have lipedema. If around 1 in 10 to 1 in 20 women have a condition, that's not "rare."
Since these figures are only guesses, they could be over-estimates, but then again they may not be counting many early cases which are hard to identify. Does every woman with a pear-shaped body have lipedema? Hard to say. Best guess is that the women with true lipedema are those with pronounced "pear" shapes and whose bottom halves put on fat in response to hormonal challenges or major stress. But what percentage of women fit this criteria is hard to say.
Because it is relatively unknown, it is common for women to go for years without being diagnosed. Women with lipedema are simply seen as fat by the public and by most doctors. Often they are pressured into diets, weight loss surgery, and/or extreme exercise to treat it. Many are shamed and mistreated due to obesity stigma and prejudice.
However, the unique pear-shaped silhouette, the sparing of the hands and feet, and the progressive nature of condition despite all attempts at diet and exercise certainly suggest that it is a real medical condition that is more complicated than "just" obesity.
Sometimes, lipedema is shrugged off as lymphedema, but the two conditions have very distinct differences. However, the lines can be blurred in the late stages because lipedema patients can develop lipo-lymphedema.
Often, lipedema patients are only diagnosed because they have been referred to lymphedema specialists who have more recognition of lipedema as a condition. By that time, however, the lipo-lymphedema has often advanced so far that the condition has become quite disabling or even life-threatening.
A significant percentage of fat people probably have lipedema and are going undiagnosed and untreated for it. This is why I want to bring particular attention to it on this blog.
This lack of recognition is probably leading to many cases of severe lipo-lymphedema that might have been prevented by having more awareness and earlier treatment of lipedema.
It is time for more care providers and consumers to learn about lipedema and how to care for it. It is time for the general public to learn about lipedema so there is less stigma attached to it. And it is time for women with lipedema to take back their power and learn to live proactively with it.
*Do you have a Lipedema story you'd like to share? Please email it to kmom AT plus-size-pregnancy dot org.  |
| Lipolymphedema |
Notice that while the woman on the left clearly has lymphedema, both legs are affected, the feet are much smaller, and there are characteristic fat pads at the knees and over-shouldering around the ankles. This is a LIPEDEMA patient who has also developed secondary lipo-lymphedema.
When lipedema patients develop significant secondary lymphedema, it can become very extreme and debilitating, even life-threatening. The goal of diagnosis and treatment of lipedema is to keep it from progressing to these severe stages.
Summary
Lipedema was first described in the medical literature in 1940 by Doctors Allen and Hines of the Mayo Clinic. However, it did not become well-known among U.S. providers. European providers were also slow to recognize lipedema, but generally have more awareness of it today than U.S. providers. Many countries outside of Europe and the U.S. have even less awareness of it.
One important point is that we do not truly know how common lipedema is. It is called a "Rare Adipose Disorder" but it is probably not that rare. The Lipoedema Australia Support Society (LASS) says that 5-15% of women may have it. One epidemiological study estimated that about 11% of women have lipedema. If around 1 in 10 to 1 in 20 women have a condition, that's not "rare."
Since these figures are only guesses, they could be over-estimates, but then again they may not be counting many early cases which are hard to identify. Does every woman with a pear-shaped body have lipedema? Hard to say. Best guess is that the women with true lipedema are those with pronounced "pear" shapes and whose bottom halves put on fat in response to hormonal challenges or major stress. But what percentage of women fit this criteria is hard to say.
Because it is relatively unknown, it is common for women to go for years without being diagnosed. Women with lipedema are simply seen as fat by the public and by most doctors. Often they are pressured into diets, weight loss surgery, and/or extreme exercise to treat it. Many are shamed and mistreated due to obesity stigma and prejudice.
However, the unique pear-shaped silhouette, the sparing of the hands and feet, and the progressive nature of condition despite all attempts at diet and exercise certainly suggest that it is a real medical condition that is more complicated than "just" obesity.
Sometimes, lipedema is shrugged off as lymphedema, but the two conditions have very distinct differences. However, the lines can be blurred in the late stages because lipedema patients can develop lipo-lymphedema.
Often, lipedema patients are only diagnosed because they have been referred to lymphedema specialists who have more recognition of lipedema as a condition. By that time, however, the lipo-lymphedema has often advanced so far that the condition has become quite disabling or even life-threatening.
A significant percentage of fat people probably have lipedema and are going undiagnosed and untreated for it. This is why I want to bring particular attention to it on this blog.
This lack of recognition is probably leading to many cases of severe lipo-lymphedema that might have been prevented by having more awareness and earlier treatment of lipedema.
It is time for more care providers and consumers to learn about lipedema and how to care for it. It is time for the general public to learn about lipedema so there is less stigma attached to it. And it is time for women with lipedema to take back their power and learn to live proactively with it.
Resources and References
Resources
*Trigger Warning: Many of these sites are not size-friendly. However, because they also contain valuable information about lipedema and its treatment, they are included here.
Resources
*Trigger Warning: Many of these sites are not size-friendly. However, because they also contain valuable information about lipedema and its treatment, they are included here.
- http://www.curelipedema.org/# - Cure Lipedema
- http://www.lipomadoc.org/lipedema.html - Website of Karen L. Herbst, PhD, MD, one of the most pre-eminent researchers on lipedema. She is an endocrinologist practicing in Arizona
- http://fatdisorders.org/fat-disorders/lipedema-lipoedema-description - Website of the Fat Disorders Research Society
- http://www.lipv.nl/Lipedema%20a%20frequently%20misdiagnoseds%20and%20misunderstood%20syndrome.pdf - Educational article on lipedema for care providers, good but technical in parts. (Not size-friendly; advocates "rigorous" weight control and suggests bariatric surgery)
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309375/ - United States National Library of Medicine, National Institutes of Health
- http://en.wikipedia.org/wiki/Lipedema - Wikipedia article on lipedema
- http://www.nhs.uk/conditions/lipoedema/Pages/Introduction.aspx - United Kingdom's NHS website page on Lipedema
- http://www.lymphedema-therapy.com/Lipedema.htm - Lymphedema Therapy website
- http://www.hanse-klinik.de/englisch/Lipoedema.pdf - article on lipedema from one of the foremost clinics in Germany that treats lipedema
- http://www.lymphedema.com/lipedema.htm - Peninsula Medical summary of lipedema
- http://www.lymphedemapeople.com/wiki/doku.php?id=lipedema - Lipedema page from a website specializing in lymphedema information (Lymphedema People)
- http://www.webmd.com/women/guide/lipedema-symptoms-treatment-causes - WebMD article
- http://www.lipedemaliposuctioncenter.com/about-lipedema.html - Liposuction clinic specializing in lipedema patients
- http://www.lymphedemablog.com/2012/12/13/a-closer-look-at-lipedema-and-the-effects-on-the-lymphatic-system/ - Effect of lipedema on the lymphatic system
- Differential Diagnosis for lipedema vs. lymphedema - how to differentiate these conditions
- http://rlbatesmd.blogspot.com/2010/02/lipedema-lymphedema-lipolymphedema.html - blog entry on lipedema vs. lymphedema, written by a plastic surgeon
- http://www.mdjunction.com/forums/dercums-disease-discussions/articles/2888889-lipolymphedema-dercums - details about lipedema and lymphedema
- http://www.thelymphoedemacliniclondon.co.uk/pages/treatment-for-lipedema-and-lipo-lymphoedema.php - treatment options for lipedema and lymphedema
- http://blog.wegohealth.com/2014/09/15/the-phases-of-a-lipedema-diagnosis/ - Guide to navigating a lipedema diagnosis, written by Sarah Bramblette, a prominent lipedema activist
- http://lipedema-simplified.org/ - blog and advocacy from Catherine Seo, who is dealing with lipedema and who is the maker of the new film "Born To Be Fat" about lipedema. (Caution, weight loss and diet talk, but still a worthwhile resource for Fat-Acceptance folk)
- lipladyfab.wordpress.com - blog of woman dealing with lipedema and undergoing liposuction
- http://www.biglegwoman.com - blog of woman dealing with lipedema
- http://born2lbfat.com/category/livingwithlipedema/ - blog of woman dealing with severe lipedema, including her journey with gastric bypass
- http://lipedemagirl.tumblr.com/me - tumblr account of a woman dealing with lipedema and lymphedema, including having had lap band surgery
- Big Fat Legs http://www.bigfatlegs.com/ - blog of woman dealing with lipedema
- Lipoedema Ladies (U.K.) - http://www.lipoedemaladies.com/ - U.K. support group for lipedema
- http://www.tillysmidt.nl/LIPEDEMA_Englisch_for_Lipoedeem.html - website of Dutch woman with lipedema who was an early voice for treating lipedema (not a size-friendly resource)
- https://www.facebook.com/lilithnixroadtorecovery/posts/537379969717549 - Facebook page of a woman with lipo-lymphedema (this link takes you to her biography and lipedema story)
- http://www.thedoctorstv.com/videos/living-with-lymphedema-and-lipedema - video biography of Sarah from "The Doctors" episode (she has stage 4 lipolymphedema)
- http://www.nursevirginiablog.com/?s=lipedema - Nurse Virginia's blog (not size-friendly)
- https://mylipedemajourney.wordpress.com/ - a thin woman's journey with lipedema and tumescent liposuction to treat it
- http://www.lass.org.au/ - Lipoedema Australian Support Society (LASS)
- http://www.talklipoedema.org/ - U.K. support and information group for lipedema
- https://livingwithlipoedema.wordpress.com/ - a British woman's journey with lipedema, particularly focusing on its emotional effect and the treatments she has tried
- http://www.laurajdavis.com/blog/category/lipolymphedema - one woman's history of lipo-lymphedema, failed attempts at weight loss, and treatment difficulties
Med Hypotheses. 2014 Aug 23. pii: S0306-9877(14)00295-3. doi: 10.1016/j.mehy.2014.08.011. [Epub ahead of print] Pathophysiological dilemmas of lipedema. Szél E1, Kemény L2, Groma G2, Szolnoky G2. PMID: 25200646
Lipedema is a common, but often underdiagnosed masquerading disease of obesity, which almost exclusively affects females. There are many debates regarding the diagnosis as well as the treatment strategies of the disease. The clinical diagnosis is relatively simple, however, knowledge regarding the pathomechanism is less than limited and curative therapy does not exist at all demanding an urgent need for extensive research. According to our hypothesis, lipedema is an estrogen-regulated polygenetic disease, which manifests in parallel with feminine hormonal changes and leads to vasculo- and lymphangiopathy. Inflammation of the peripheral nerves and sympathetic innervation abnormalities of the subcutaneous adipose tissue also involving estrogen may be responsible for neuropathy. Adipocyte hyperproliferation is likely to be a secondary phenomenon maintaining a vicious cycle. Herein, the relevant articles are reviewed from 1913 until now and discussed in context of the most likely mechanisms leading to the disease, which could serve as a starting point for further research.











20 comments:
I have learned so much from your blog. You cover topics that no one else is talking about, and in incredible depth at that. I just wanted to say a quick 'thanks' for the time and effort you put into writing!
I think I have this, as I have the "bracelet" at the ankles. I've tried to get a compression stocking, as I thought it was fluid problems and nerve damage due to a fall down a staircase where I landed face front on the legs (I was carrying a big box and landed on that, so my head and torso were spared). My legs turned black for several months, and I've had mystery pains (I thought they were ghost pains) in the leg, a bump forming below the knee (but only on one leg), and extreme pain during massages and shaving.
The nurses at the home care store wanted to help me, but of course my leg is bigger than size L, so I was to go and get a prescription. I didn't because I knew that my doctor wouldn't give me one. I've since stopped going to him.
I think I also have the lipolymphedema as when I go to bed my legs are twice they size they are as when I wake up in the morning. I also don't have 100 trips to the bathroom in the night, usually just one, since I drink some water or milk before bed.
I will print this out and take it to the doctor, as well as some "authority" entry on it, with my symptoms listed. All the doctors seem to want to do with me is bariatric surgery.
If you have it, I am so happy that this will help you figure it out and get diagnosed. Be aware that many docs know nothing about it so you may have to do some educating and advocating for yourself to know for sure.
See the next post coming up on the stages and types of lipedema. In the early stages, there can be a lot of edema that builds up by the end of the day and resolves overnight or upon rest and elevation. In the later stages, it doesn't usually resolve as much, so you may not have lipolymphedema after all.
I'm still researching the treatments, but from what I've read so far, only certain types of compression garments are suitable for lipedema. The ones for lymphedema tend to be too strong (and thus painful) and made in the wrong way for treating lipedema. More info on that to come later in the series.
Hi, I love your writing style. You write clearly and explain things well. Your blog is everything I would want a blog of mine to be if I had the gumption to organize and edit. Great job! Now I can send folks to you and don't have to do it myself.
Hi, is there a certain age you recognize you have it? And will excercise (any form) help in any way
Anna's Life, the progress of lipedema varies greatly from one person to another. Typically it gets much worse and really recognizable in a person's 40s and 50s. They had it previously, but not always so distinctively that people not very familiar with lipedema would be able to say for sure that was it. However, there are some women who have it pretty badly in their late 30s, even 20s. It often first really shows strongly in a person's teens, but the course of how it progresses really varies from person to person.
If you have read my blog posts on lipedema treatment, you will know that exercise is actually quite important in helping with lipedema. The lymph system does not have a "pump" (like the heart is a pump for the blood system); it depends on exercise to help the lymph fluids circulate efficiently. Exercise won't cure lipedema, mind, but it is helpful in treating it and trying to keep it from getting too much worse.
As June is Lipedema Awareness Month, may we share your blog with our friends on FB? They are very well written, documented and illustrated!! Of course, you would get the credit for creating these very helpful masterpieces!!
Yes, as long as it's credited properly, please do share it! Don't forget I also have a Facebook page now too. We need to get the word out about lipedema!
I have lipedema and it has psychological effects as well. People are cruel to those who have "freak" bodies. They don't understand that some of us have diseases that make us the way we are. When I first saw a picture of my legs on someone else's body, I cried. I feel better that I know more about lipedema. Thanks for your site.
I am so glad to find your explanation of Lipedema. I am 74 yrs old and have this plus Systemic Mastocytosis, which is also a rare condition. I started my married life as a 100 lb 20 year old, but have gained weight through 3 pregnancies, and several surgeries during my lifetime. The Mastocytosis and Spinal stenosis in the lumbar region make exercise difficult, but I will still look forward to reading your advice and doing whatever is possible to feel better.
Thank you so very much for this very well-written and important blog. My mother is 90 and has both lipedema and lymphedema which no doctor had diagnosed until just a few months ago when she also developed a blood clot in her leg. I have lipedema and have struggled to lose weight and inches for years. Recently I had to self-diagnose my Dercum's Disease, after seeing at least six different doctors and having neither the lipedema not the Dercum's diagnosed. The medical profession in the U.S. is downright deplorable, allowing so many people to suffer needlessly and to go without therapies that might slow or halt the progression of these diseases. All of these doctors who blithely recommend exercise and changing one's diet while being blind to these illnesses should be profoundly ashamed of their collective ignorance. I've been subjected to far too many medical "professionals" (and I use the term very loosely) who display arrogance and condescension while they are basically botching their diagnoses -- I have no mercy with these idiots any longer. Why are we paying so much for healthcare and getting uneducated guesses about our illnesses? It's a complete travesty.
Whew! So sorry for the rant, but it feels good to get that off my chest!
My sister and I live in South Africa and developed lipedema at puberty on the lower legs. We inherited this condition from our paternal grandmother who eventually had her legs amputated at age 71 due to complications from the lipedema, mainly because of the lack of circulation. She was housebound for years and had much pain, and spontaneous bruising with spider veins.
She died of shock from the operation.
My sister and I from puberty had pain from the slightest pressure on our lower legs and would not let anyone touch them. We have always hated our ugly legs particularly since we dieted constantly and followed a healthy regimen to keep our weight down. We were thin, apart from our lower legs, and the feet were also dry thin, with the characteristic band you speak of. We never had ankles to show off due to this condition.
I am now 66 years old, twenty years ago we were on holiday in Israel and I suffered so much pain from walking and the pain didn't go away and a whole lot of spider veins appeared. I also had the condition on and above the knees. The spider veins appeared above the knees too. I also could not wear trainers because I could never bend the foot in them due to the fat behind the ankle.
On my return I went to have liposuction on my knees and ankles, removing two liters of pure fat. This helped a lot and I could then wear trainers.
I still deposited more fat even though the surgeon said it would never come back because the fat cells were gone, and he told me that it was impossible to give me attractive ankles though that was not my motivation. I just realized that if I didn't do something I would end up like my grandmother , who had died in England, having lived there all her life.
I am now considering going for liposuction again. The spontaneous bruising is constant and when it fades very often leaves new spider veins.
If you don't have lipedema you have no idea of the pain of this condition. Also the pains in the legs themselves now that I didn't have when I was young, which occur when walking for more than about 15 minutes.
My thin feet just look silly.
I am glad this condition now has a name. We thought we were freaks and always wore long dresses to cover it up.
I am a size 14/16 on top and a size 24 on the bottom. The diameter of my ankles is over 5 inches. Visibly it looks like I have Lipedema. But I don't bruise easy, and I do not experience pain in my legs, even with pressure. Is it possible too have Lipedema without the pain?
Dear Wellrounded mama,
as far as I can see you are using one of our picutures without permission - (blue Background, black underwear).
you can use it furher if you would make a link to our Website - www.lymphedema-clinic.com .
Thank you in advance.
Andreas Wittlinger
CEO Lymphedema Clinic Wittlinger Walchsee/Austria
Thank you so much for your hard work and dedication! I have been having trouble for years but nobody knew what was going on saying I was obese with poor circulation. I once read about Dercums Disease, talked to my doctor who didn't know what I was talking about. Finally in 2007 I had gastric bypass surgery and happily lost 140 lbs but then started gaining & I'd go back on my bariatric diet and nothing. Fast forward 10 years & a bariatric revision later, I start gaining 5-7 lbs every week. Scared I went to my doctor who sent me to another who sent me to another, finally landed at a Nephrologist, he looked at me and asked why I was there. He said he'd love to be able to treat me but that he was the wrong doctor and he sent me to a specialist who took one look at me and said, you have a Lipedema & Lymphedema. My mom was with me & he looked over at her and said, and you do too! What's funny is that my grandmother had "poor circulation" with seeping and the doctor put some lotion on her legs and wrapped them. My mother had "poor circulation" and some seeping and her doctor put medicated lotion on her legs, wrapped them twice a week for 4 years. She's been good for 5 years now. So then it's my turn, although I don't have the seeping, but I gained 80 lbs from September to January. I was put on 2 water pills, had physical therapy, wear compression stockings & im to get more coverage so looking for a "body suit"...any good ideas? I'm having Liposuction surgery next month, my left hip is much larger than my right. I just hope it works. Most of my weight gain and swelling was from my waist down. Now I'm noticing my arms are swelling along with my hands/fingers. Will this ever end? I pray that the surgery wil be a success. Again, thanks so much for all of your information!!! ❤️
Thank you for the concise info & your time to blog this awareness of Lipedema & the differences between Lymphedema. And the personal determination to find a medical professional for diagnosis. I had a very aware oncologist to direct me & my treatment of Lymphedema fast & effectively. God bless everyone.
This. Exactly this for me.
I believe I have had this since I was 18, I am now 53. At 21 my upper thighs and upper arms started to gain disproportionately to my very slight somewhat underweight frame. At 22 I had my tonsils out with excessive bleeding and had to go on steroids and an extra long recovery with liquid diet. I went from a size 5 to size 22 in a matter of four months! All of the weight seemed to be in my belly, upper legs and upper arms and was very lumpy. No matter how much dieting I did it wouldn't come off. I suddenly became off balance,like I was walking through quicksand and uncoordinated. My arms and legs hurt. I didn't dare complain, I was just overweight and needed to eat less and exercise. I heard it over and over. Except I was practically an anorexic. I finally found a Dr. 4 years ago who actually listened and put me on a gluten free diet and the a good deal of the weight came off except my upper arms and upper legs and belly were still holding enough to keep me overweight. I said something to him about a month ago that the fat that was left was painful....He said why didn't you tell me that a long time ago, you could have this rare disease called Dercums or lipidema I must do some research. I go back in two weeks to discuss with him. But after looking on this site, I'm sure that's what it is. I'm so hopeful there is help! I'm so tired of living like this.
This link didnt work: http://www.hanse-klinik.de/englisch/Lipoedema.pdf - article on lipedema from one of the foremost clinics in Germany that treats lipedema
I was diagnosed with Mantle Cell cancer in 2018. In six weeks on Rituxin-Benemussin I gained 47 pounds. I slept all the time. The cancer is of the lymph system. In December of 2018 -I suddenly grew a large fat tumor on each side of my buttock near the waist.Surgery on one side showed no cancer but the doctor diagnosed Dercums. It was understood I was basically allergic to Rituxin . But now I knew why I developed a ski jump rear and two very large upper arms at 65 years! My right leg became larger.
That became lymphadema. I had wrapped my legs from 18 years old on during pregnancies. I was investigated for kidney problems with multiple surgerys. I then started fluid gains each month at midcycle. My abdomen filled with fluid after hiking.
After my fourth child-nothing would remove the extra 14 pounds .My fifth child I dieted and did not gain a pound Unfortunately the doctor created a mess and a hysterectomy followed and four years of tissue removal and many bowel obstructions. At times on NG tubes for over a month and never one pound lost! hashimotos started. then a sudden 30 lbs
in less than 3 weeks. Severe diets and aggressive exercise.Then 40 lbs! and Lymes ! Now I had 7 surgeries for spinal stenosis of cervical and lumbar that I was born with plus radiation of thoracic spine. Many fat tumors in spinal areas that added to pain. Another 40 lbs but this I fight up and down for 30 years. I swam and exercised daily in the pool, rode a bike walked many miles.The emmotional pain of holding ones head high and surviving the cruel taunts and remarks and staying
upbeat and kind in heart and mind helped. I kept many journals of my meals for years. The pain in my spine, legs is
extreme. I have 5 auto immune conditions now. The lymph nodes are cancer free this year still ! I must keep my legs up so as to avoid debilitating pain.
Information like this has given me hope and justice.
I love listening to Kathy Bates bring light to the lymphadema part .
At 74-I hope to bring some of this in control with procedures that remove and restore.
Thank you!!!!
Oklahoma has only one doctor supposedly have ing insight but since his report said "obese due to excessive calorie intake" without speaking to me than -obviously his understanding is not acceptable.
In 2021 I had a knee restoration which blew up my right leg and has brought on horrible leg problems.
Post a Comment